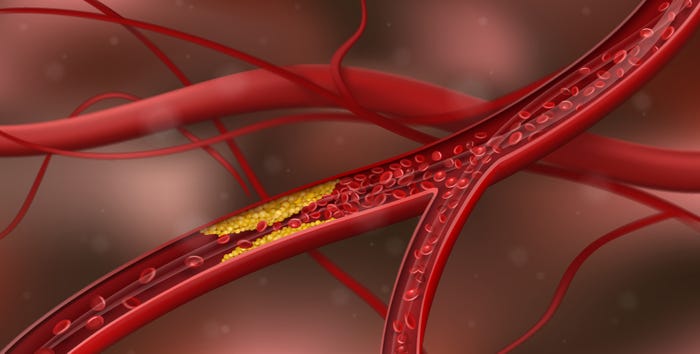
Heart Health
Young at heart: Meeting demand for supplements that support heart health
Sponsored Content
Young at heart: Meeting demand for supplements that support heart health – product development guideYoung at heart: Meeting demand for supplements that support heart health – product development guide
Heart health is a strong, growing category. Stay on top of consumer priorities and the most efficacious ingredients to address them.
Subscribe and receive the latest insights on the health and nutrition industry.
Join 37,000+ members. Yes, it's completely free.







































.png?width=800&auto=webp&quality=80&disable=upscale)