Vitamins
thumbnail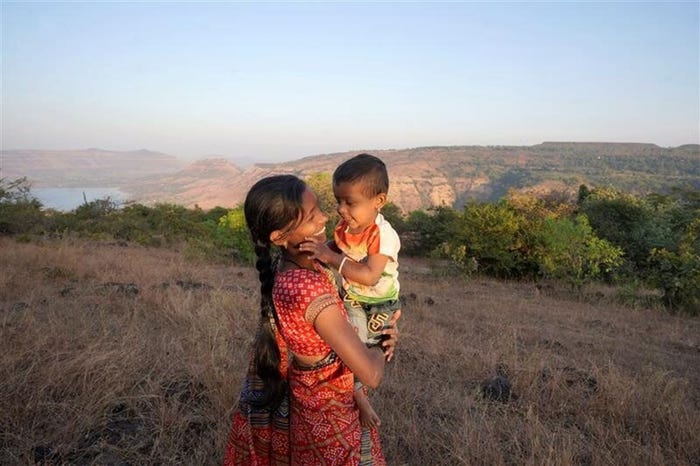
Supplements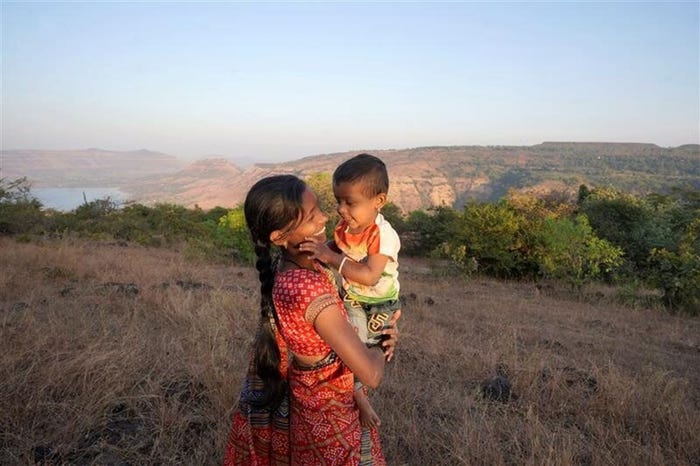
30 years strong: Support Vitamin Angels' mission to end child malnutrition30 years strong: Support Vitamin Angels' mission to end child malnutrition
Howard Schiffer had an aha moment that would bring him to his life’s mission.
Subscribe and receive the latest insights on the health and nutrition industry.
Join 37,000+ members. Yes, it's completely free.










.png?width=300&auto=webp&quality=80&disable=upscale)


































.png?width=800&auto=webp&quality=80&disable=upscale)