Bending the Rules
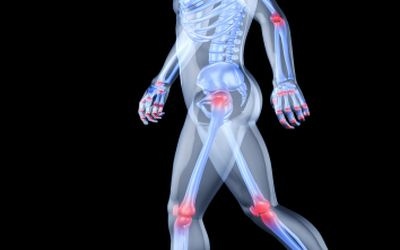
Keeping joints healthy and ready to tackle everyday bends and high-impact sports
Highlighted Ingredients for Joint Health |
|
As well studied as the human body is, scientists have not come to a general decision on the number of joints in the body. Even with a simple definitiona joint is the location where two or more bones make contactno definitive answer has been determined. Because skull bones knit together in a way that makes them permanently fused, many view them as a single unit; however, others consider them joints. Take those conjunctions, plus the fact that the number of bones in a body changes with age as they fuse together, and the total number of joints in the average human is elusive.
A good guess is from the mid-200s to mid-300s, all working together with bones and muscles to allow us to move and function in everyday activities from finding a more comfortable sleeping position and playing Frisbee with the dog. However, with so many joints fulfilling lifes expectations, chances are high they will bring pain to a person a few times in the lifespan.
All types of connections can be damaged with inflammation, mostly due to a form of arthritis. Joint damage caused by physical trauma may not initially be arthritis, but this type of injury may develop into the disease. Arthritis involves the breakdown of cartilage; without the normal amount of cartilage, bones rub together, causing pain, swelling and stiffness.
Of the 100 types of arthritis, osteoarthritis (OA) is the most common, but gout and rheumatoid arthritis (RA) are other common forms. OA is caused by wear and tear on a joint, according to the National Institutes of Health (NIH). After cartilage breaks down, bony spurs or extra bone may form around the joint, and the ligaments and muscles around the joint become weaker and stiffer. Often, the cause of OA is unknown, but it is related to aging. The symptoms of OA usually appear in middle age, and almost everyone has some symptoms by age 70. Before age 55, OA occurs equally in men and women. After age 55, it is more common in women.
RA is an autoimmune disease, which means the body's immune system mistakenly attacks healthy tissue, and it can occur at any age, but is more common in middle age. RA usually affects joints on both sides of the body equally. Wrists, fingers, knees, feet and ankles are the most commonly affected.
According to the NIH, the goal of arthritis treatment is to reduce pain, improve function and prevent further joint damage. The underlying cause cannot usually be cured. Americas medical research agency said lifestyle changes are the preferred treatment for OA and other types of joint inflammation. Exercise can help relieve stiffness, reduce pain and fatigue, and improve muscle and bone strength. The NIH also recommends getting eight to 10 hours of sleep each night, avoiding staying in one position for too long, practicing stress-reducing activities, and eating a healthy diet full of fruits and vegetables.
Conventional treatment for joint problems includes non-steroidal anti-inflammatory drugs (NSAIDs); however, they can come with unwanted side effects. In 1998, a study from Stanford University of Medicine, Palo Alto, CA, said conservative calculations estimate approximately 107,000 patients are hospitalized annually for NSAID-related gastrointestinal (GI) complications, and at least 16,500 NSAID-related deaths occur each year among arthritis patients alone.1 In this study from the Arthritis, Rheumatism and Aging Medical Information System (ARAMIS) Post-Marketing Surveillance Program (PMS), researchers reported data from approximately 11,000 arthritis patients in the United States and Canada. Analysis of these data indicated: (1) OA and RA patients are 2.5 to 5.5 times more likely than the general population to be hospitalized for NSAID-related GI events; (2) the absolute risk for serious NSAID-related GI toxicity remains constant, and the cumulative risk increases over time; (3) there are no reliable warning signals, as close to 80 percent of patients with serious GI complications had no prior GI symptoms; and (4) independent risk factors for serious GI events were age, prednisone use, NSAID dose, disability level and previous NSAID-induced GI symptoms. The researchers noted limiting NSAID use is the only way to decrease the risk of NSAID-related GI events.
As numerous studies have shown, one way to reduce the use of NSAIDs is to supplement with natural products that address joint issues. As part of its nutrient recommendations, NIH said vitamin E and omega-3 essential fatty acids (EFAs) in the diet can help aid arthritic conditions. It also recommended applying capsaicin cream topically over painful joints to provide relief in three to seven days.
Of course, those arent the only ingredients that can help the joints function optimally, and one doesnt have to wait until arthritis kicks in to find joint help. As many Baby Boomers are getting older, they may want to address joint pain that comes from general wear and tear, and even younger consumers of the athletic persuasion may look to reduce inflammation in between training sessions.
Natural ingredients generally address joint pain in one of two ways: they either try to build the cartilage that's been destroyed or they focus on reducing the inflammation that comes from bones rubbing together. Both tactics have shown to be effective in reducing pain in clinical trials.
Next Page: Glucosamine and Chondroitin Sulfate
Bonus: Chart - Round Up of Joint Health Ingredient Studies
Glucosamine, Chondroitin Sulfate
The two best-known natural ingredients for joint health are glucosamine and chondroitin sulfate, which have shown benefits when taken separately, but have shown even more benefit when taken together. The NIH said glucosamine and chondroitin sulfate may help control pain in OA patients, although they do not seem to help joints grow new cartilage. NIH noted some doctors recommend a trial period of three months to see whether glucosamine and chondroitin work.
The amino sugar glucosamine is a precursor for glycosaminoglycans (GAGs). As GAGs are a major component of joint cartilage, the theory is supplemental glucosamine may help to prevent cartilage degeneration and may help new cartilage grow. The body produces glucosamine and distributes it in cartilage and other connective tissues.
A 2001 study reported gluosamine sulfate could be a disease-modifying agent in OA, as knee OA patients who took a glucosamine preparation, used exclusively in the prescription medicine made by Rotta Pharmaceutical Co., for three years had no significant joint-space loss compared to those in the placebo group, who had progressive joint-space narrowing.2 Further, symptoms worsened slightly in patients on placebo compared with an improvement observed after treatment with glucosamine sulfate, as assessed by Western Ontario and McMaster Universities (WOMAC) OA index scores.
A 2007 Spanish study found 1,500 mg/d of glucosamine sulfate was more effective than placebo, and worked as well the drug acetaminophen, in treating knee OA symptoms.3 And a 2006 review of 20 randomized controlled trials (RCTs) evaluating the effectiveness and toxicity of glucosamine in OA found studies using Rotta Pharmaceutical's glucosamine showed it was superior to placebo in the treatment of pain and functional impairment resulting from symptomatic OA; however, results from studies using a non-Rotta preparation failed to show benefits in pain and WOMAC function.4 WOMAC outcomes of pain, stiffness and function did not show a superiority of glucosamine over placebo for both Rotta and non-Rotta preparations of glucosamine.
But its not news that glucosamine study results vary greatly. A 2007 investigation from Boston University Medical Center evaluated 15 glucosamine trials and reported heterogeneity among trials of glucosamine is larger than would be expected by chance.5 The potential explanations they found included different glucosamine preparations, inadequate allocation concealment and industry bias.
Glucosamine's "sister" ingredient, chondroitin sulfate, a sulfated GAG, is a complex carbohydrate that helps cartilage retain water. In 1998, a multicenter, randomized, double blind, controlled French study indicated chondroitin sulfate at 1,200 mg/d improved joint mobility in patients with mono or bilateral knee OA.6 Oral chondroitin sulfate decreased pain and improved knee function in a 2004 study, which found a three-month intermittent administration of 800mg/d twice a year supported prolonged effects for patients with OA.7
A meta-analysis of seven controlled clinical trials of chondroitin sulfate in the treatment of OA found it may be useful, but recommended further investigations in larger cohorts of patients for longer time periods.8 The studies, which followed patients for 120 days or longer, showed chondroitin sulfate was significantly superior to placebo with respect to the Lequesne index, a popular assessment used to determine functional ability in OA patients, and pain Visual Analogue Scale (VAS), which tracks pain on a continuum. Data showed at least 50-percent improvement in the study variables in the chondroitin sulfate groups compared to placebo.
Research on the ingredients alone may not prove to be as stellar as the combination. A World Health Organization (WHO) review in 2007 evaluated published studies of the effect of glucosamine salts and chondroitin sulfate preparations on the progression of knee or hip OA.9 On the basis of the results of recent RCTs and meta-analyses, the study concluded glucosamine sulfate (but not glucosamine hydrochloride) and chondroitin sulfate have small-to-moderate symptomatic efficacy in OA, and compelling evidence shows glucosamine sulfate and chondroitin sulfate may interfere with progression of OA. However, in the review, researchers noted the controversy regarding the efficacy of these agents with respect to symptomatic improvement remains, despite multiple double blind, controlled clinical trials. They said the seemingly contradictory results may be due to several potential confounders, including placebo response, use of prescription medicines versus over-the-counter (OTC) pills or food supplements, or use of glucosamine sulfate versus glucosamine HCL.
The biggest test on the effects of glucosamine and chondroitin sulfate for the treatment of knee OA came with the Glucosamine/Chondroitin Arthritis Intervention Trial (GAIT), the first large-scale, multicenter clinical trial in the United States looking at these supplements' effects on arthritis, did not show the results many in the natural products industry wished to see.10 The University of Utah School of Medicine, Salt Lake City, coordinated this study, which was conducted at 16 rheumatology research centers across the United States. The National Center for Complementary and Alternative Medicine (NCCAM) and the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), two components of the NIH, funded GAIT. In this 24-week trial, patients either took glucosamine alone at 1,500 mg/d, chondroitin sulfate alone at 1,200 mg/d, glucosamine plus chondroitin sulfate combined at 1,500 mg and 1,200 mg/d respectively, or the prescription drug celecoxib at 200 mg/d. Participants taking the positive control, celecoxib, experienced statistically significant pain relief versus placebo; about 70 percent of those taking celecoxib had a 20-percent or greater reduction in pain versus about 60 percent for placebo. However, the researchers reported no significant differences between the other treatments tested and placebo.
For a subset of participants with moderate-to-severe pain, glucosamine combined with chondroitin sulfate provided statistically significant pain relief compared with placeboabout 79 percent had a 20-percent or greater reduction in pain versus about 54 percent for placebo.11 According to the researchers, because of the small size of this subgroup, these findings should be considered preliminary and need to be confirmed in further studies. For participants in the mild pain subset, glucosamine and chondroitin sulfate together or alone did not provide statistically significant pain relief.
While the GAIT trials initial results were for the first 24 weeks of the intervention, the study subjects continued their supplements for two years.12 The Salt Lake City researchers reported, compared with placebo, the odds of achieving a 20-percent reduction WOMAC pain after two years were celecoxib: 1.21, glucosamine: 1.16, combination glucosamine/chondroitin sulfate: 0.83 and chondroitin sulfate alone: 0.69, but were not statistically significant. Therefore, no treatment, including the prescription drug, achieved a clinically important difference in WOMAC pain or function as compared with placebo. However, glucosamine and celecoxib showed beneficial, but not significant, trends.
Next Page: Hyaluronic Acid and Collagen
Bonus: Chart - Round Up of Joint Health Ingredient Studies
Hyaluronic Acid
Another GAG, hyaluronic acid (HA) has been used as an injection for the treatment of OA for more than 15 years,13 but recent evidence has looked at its ability to treat joint health using other delivery systems. Hyal-Joint from Bioiberica is one particular branded ingredient that has oral-delivery scientific backing. A pilot clinical trial showed daily supplementation with oral HA from a natural extract of chicken combs (Hyal-Joint) was useful to enhance several markers of quality of life in adults with OA of the knee, such as the WOMAC score for physical function and total symptoms, as compared to placebo.14
And Hyabest®(J) from Kewpie Corp. affected significant improvement in WOMAC scores after four weeks of oral intake.15 In the study, the placebo group also showed a decline in WOMAC scores, but it was not statistically significant. In the analysis of the scores of patients suffering from severe pain, the Hyabest (J) group showed significant improvement over the placebo group.
Collagen
The breakdown of collagen causes pain, so adding more should in theory reduce inflammation. And perhaps, its not just theory. A 1998 study showed oral administration of cartilage-derived type-2 collagen showed beneficial effects on RA pain management at the lowest dose tested (20 mcg/d) for 24 weeks.16 And oral chicken type-2 collagen was shown to be a safe and effective therapy for juvenile RA in a 12-week study involving 10 patients.17 Eight patients had reductions in both swollen and tender joint counts after three months of supplementing with collagen. The mean changes from baseline in swollen and tender joint counts for the eight responders at the end of the study were 61 percent and 54 percent, respectively.
UC-II®, a patented undenatured type-2 collagen ingredient from InterHealth Nutraceuticals, has been tested clinically in a randomized, double blind trial, which showed 40 mg/d of UC-II increased joint comfort, flexibility and mobility.18 UC-II was more effective than 1,500 mg/d of glucosamine combined with 1,200 mg/d of chondroitin; a 40-mg daily dose of UC-II was more than two times as effective as 2,700 mg/d of glucosamine combined with chondroitin in promoting complete joint health. It outperformed the glucosamine/chondroitin combination using three different assessment tools: WOMAC, VAS and Lequesne functional index. UC-II also significantly reduced pain during daily activities, including walking on a flat surface, performing heavy domestic duties, ascending stairs and while resting in bed.
A pilot study conducted for 42 days found UC-II (10 mg/d) significantly reduced pain including morning stiffness, stiffness following periods of rest, pain that worsened with use of the affected joint, and loss of joint range of motion and function in five female subjects (58 to 78 years) suffering from significant joint pain.19
And arthritic dogs also benefited from daily treatment of with UC-II in a study from 2005.20 Dogs receiving 1 mg or 10 mg UC-II/d for 90 days showed significant declines in overall pain and pain during limb manipulation and lameness after physical exertion, with 10 mg showing greater improvement. In addition, dogs receiving UC-II for 90 days showed increased physical activity level. Following UC-II withdrawal for a period of 30 days, all dogs experienced a relapse of overall pain, exercise-associated lameness and pain-upon-limb manipulation.
Adding UC-II to glucosamine and chondroitin offered even more benefit to arthritic dogs. In one study, dogs receiving UC-II alone showed significant reductions in overall pain within 30 days (33 percent) and pain upon limb manipulation and exercise-associated lameness after 60 days (66 percent and 44 percent, respectively) of treatment.21 Maximum reductions in pain were noted after 120 days of treatment (overall pain reduction, 62 percent; pain reduction upon limb manipulation, 91 percent; and reduction in exercise-associated lameness, 78 percent). The overall activity of the dogs in the UC-II supplemented with glucosamine and chondroitin group was significantly better than the glucosamine plus chondroitin-supplemented group. Glucosamine and chondroitin alleviated some pain, but in combination with UC-II, provided significant reductions in overall pain (57 percent), pain upon limb manipulation (53 percent) and exercise-associated lameness (53 percent). Following withdrawal of supplements, all dogs experienced a relapse of pain.
BioCell Collagen®, a dietary ingredient that is a naturally occurring matrix whose three major constituents, collagen type 2, chondroitin sulfate and HA, are reduced to highly bioavailable, low-molecular weight forms using a patented hydrolysis process, is made from articular cartilage, and BioCell Technology said its composition is similar to that of human articular joint cartilage.
In 2010, a multicenter, double blind, placebo-controlled, unpublished trial demonstrated the safety and efficacy of BioCell Collagen in addressing OA symptoms and in improving various physical activities, as measured by VAS and WOMAC scores. A previous unpublished 16-patient study of BioCell Collagen demonstrated a safety profile and statistically significant efficacy in supporting chronic degenerative joint conditions in patients with OA.
Next Page: Omega-3s
Bonus: Chart - Round Up of Joint Health Ingredient Studies
Omega-3s
EFAs are known for their anti-inflammation properties, so its no surprise they aid joint health. Marine oils contain two polyunsaturated omega-3 fatty acids, eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). Both fatty acids possess anti-inflammatory effects; however, because EPA has a similar chemical appearance as arachidonic acid (AA)which has pro-inflammatory effectssome believe it can better reduce inflammation because it displaces AA from the phospholipid membranes of tissues and cells.
Following this theory, EPAX AS markets a high-EPA fatty acid fish oil formula, 4510 TG, with 90 mg/g EPA and 70 mg/g DHA. A 12-week, double blind, randomized study on this formula reported dietary supplementation with fish oil (3.6 g/d of omega-3 EFAs) resulted in significantly reduced plasma Interleukin-1 (IL-1) beta levels in patients with RA.22 Interleukins of all kinds are biomarkers for inflammation. The clinical status of the patients was also improved in the fish oil group, but not in the placebo group, as judged by Ritchie's articular index.
Dietary supplementation with omega-3 polyunsaturated fatty acids (PUFAs) in patients with active RA had a modest effect on three out of eight disease variables in a multicenter, randomized and double blind study involving 51 Danish patients.23 The patients were allocated to 12 weeks of treatment with either six omega-3 PUFA capsules (3.6 g of omega-3s, from EPAX) or six capsules with a fat composition averaging the Danish diet. The researchers observed small, but significant improvements in morning stiffness, joint tenderness and C-reactive protein (CRP), an indicator of inflammation.
A similar study showed dietary supplementation with omega-3 PUFAs in RA patients improved two out of six patient-reported disease parameters in a multicenter, randomized, placebo-controlled, double blind, 12-week study. Fifty-one patients with active RA received either six omega-3 PUFA capsules (3.6 g of omega-3s, from EPAX) or six capsules with fat composition reflecting the average Danish diet.24 After the intervention, those who took the PUFAs experienced significant reductions of morning stiffness and joint tenderness.
An Australian study from 2000 reported fish oil supplementation that delivers omega-3 fatty acids at a dose of 40 mg/kg body weight/d, with dietary omega-6 fatty acid intake of less than 10 g/d, resulted in substantial cellular incorporation of omega-3 fatty acids and improvements in clinical status in patients with RA.25
Fish oil, in adequate doses, has also shown benefits to patients with ankylosing spondylitis, a long-term disease that causes inflammation of the joints between the spinal bones, and the joints between the spine and pelvis. Eighteen patients were randomized to either a low-dose (1.95 g omega-3/d, n=9) or a high-dose (4.55 g omega-3/d, n=9) supplement.26 The patients in the high-dose group exhibited a significant decrease in disease activity according to the Bath Ankylosing Disease Activity Index (BASDAI), which was not seen in the low-dose group.
And, a specialized diet that included an increased intake of fish, vitamin D and vitamin E compared to baseline significantly recuded morning stiffness, number of swollen joints, pain status and cost of medicine after six months in patients with active RA.27
Next Page: Omega-3s (cont.) and Astaxanthin
Bonus: Chart - Round Up of Joint Health Ingredient Studies
Like fish oil, krill oil offers omega-3s, but krill oils EPA and DHA are hooked in a double-chain phospholipid structure. In fish oil, these omega-3 fatty acids are found in the triglyceride form. The phospholipid structure of the EPA and DHA in krill oil makes them more absorbable and allows for an easier entrance into the mitochondria and the cellular nucleus. A 2010 study found krill oil offers more omega-3s than a comparable amount of fish oil.28 Perhaps its this increased amount of omega-3s that allows krill oil to have a beneficial effect on arthritis. A study on krill oil (as Neptune Krill Oil, NKO, from Neptune Technologies & Bioressources) found a dose of 300 mg/d significantly inhibited inflammation and reduced arthritic symptoms within a seven- and 14-day treatment.29 The randomized, double blind, placebo-controlled study included 90 patients with confirmed diagnosis of cardiovascular disease (CVD) and/or RA and/or OA and with increased levels of CRP (greater than 1 mg/dl). One group of patients received NKO (300 mg/d) and another group received a placebo. After seven days of treatment, NKO reduced CRP by 19.3 percent compared to an increase of 15.7 percent observed in the placebo group. After 14 and 30 days of treatment, NKO further decreased CRP by 29.7 percent and 30.9 percent respectively. The CRP levels of the placebo group increased to 32.1 percent after 14 days and then decreased to 25.1 percent after 30 days. The between group difference was statistically significant at day 14 and at day 30. NKO showed a significant reduction in three WOMAC scores after seven days of treatment: NKO reduced pain scores by 28.9 percent, reduced stiffness by 20.3 percent and reduced functional impairment by 22.8 percent.
Astaxanthin
Along with other health-promoting compounds, such as phosphatidylcholine, vitamin E, vitamin A, vitamin D and canthaxanthin, krill oil also contains astaxanthin, an antioxidant that is attached to the EPA leg of the phospholipid in the krill oil. Astaxanthin is also found in other marine animals and vegetables. This red carotenoid has shown benefits to joints, even without the anti-inflammatory effects of krill oil.
In 2003, a Korean study reported astaxanthin reduced inflammatory markers in vitro.30 And a Japanese study from the same year reported astaxanthin suppressed the development of endotoxin-induced uveitis (EIU), commonly used in animals to mimic ocular inflammation in humans, in a dose-dependent fashion in rats.31
These studies showed astaxanthin can reduce inflammation in vitro and in animal models, but two studies have been conducted in humans who suffer from RA and carpal tunnel syndrome. The double blind, placebo-controlled trials were conducted by Gene Spiller, Ph.D., at the Health Research Studies Center in Los Altos, CA, and presented at the scientific meeting of the American College of Nutrition in San Antonio, Texas, in 2002. The RA clinical trial involved 21 patients with a group of 14 randomized patients consuming three astaxanthin gelcaps daily (as BioAstin, from Cyanotech Corp.) with each meal for eight weeks, and seven randomized patients consumed a placebo. Astaxanthin significant reduced pain and increased satisfaction in the ability to perform usual activities in RA patients compared to the placebo group.
The carpal tunnel syndrome clinical trial involved 20 patients with a group of 13 randomized patients consuming three astaxanthin gelcaps daily (as BioAstin) with each meal for eight weeks, and seven randomized patients consuming a placebo. Results showed a trend toward decreased wrist pain for patients consuming astaxanthin compared to the placebo group. Astaxanthin was shown to be an effective treatment for carpal tunnel syndrome, allowing patients to suffer less daytime pain with a shorter duration of pain.
Next Page: Botanicals
Bonus: Chart - Round Up of Joint Health Ingredient Studies
Botanicals
Plant compounds also offer anti-inflammatory effects, which may translate to reduced joint pain. Accumulation of AA-derived fatty acid metabolites generated via cyclooxygenase (COX-1 and COX-2) and 5-lipoxygenase (5-LOX) pathways contribute to inflammation, pain and eventual joint damage. Traditional NSAIDs favor inhibition of COX-1 over COX-2, whereas COX-2 inhibitors favor inhibition of metabolite formation from the COX-2 pathway.
Interestingly, a plant flavonoid mixture has been shown to reduce both of these proinflammatory actions at the same time. A mixed extract containing the naturally occurring flavonoids, baicalin from Scutellaria baicalensis and catechin from Acacai catechu (as Unvestin from Unigen) inhibited both COX and LOX enzymes to reduce the production of pro-inflammatory eicosanoids and attenuate edema (swelling caused by fluid in body tissues) in one in vivo model of inflammation.32 This study also found Univestin decreased gene and protein expressions of pro-inflammatory cytokines, IL-1b, IL-6 and tumor necrosis factor-alpha (TNF-a). This same flavonoid combination has also been shown to be safe for use in humans.33
A standardized bark extract of the French maritime pine Pinus pinaster (as Pycnogenol®, from Horphag Research Ltd.) is another plant compound shown to cut inflammation. It comprises of a concentration of pine bark constituents such as polyphenolic monomers, procyanidins and phenolic or cinnamic acids and their glycosides. A 2006 study provided evidence that bioavailable active principles of Pycnogenol exert anti-inflammatory effects by inhibition of proinflammatory gene expression.34 Blood samples from seven healthy volunteers were obtained before and after five days administration of 200 mg/d of Pycnogenol. Plasma samples significantly inhibited matrix metalloproteinase 9 (MMP-9) release from human monocytes and NF-B activation.
A year later, a study found Pycnogenol alleviated OA symptoms and reduced the need for NSAIDs and COX-2 inhibitors, possibly due to its antioxidant and anti-inflammatory properties.35 Thirty-seven OA patients were enrolled in a randomized, double blind, placebo-controlled trial with a parallel-group design. Patients received either placebo or Pycnogenol (50 mg tid) for three months. Patients in the Pycnogenol group experienced a significant improvement in total WOMAC score, and WOMAC subscale scores of pain and physical function at 60 and 90 days of treatment. At 90 days, significant reduction of 43 percent, 35 percent, 52 percent and 49 percent in self-reported pain, stiffness, physical function and composite WOMAC score, respectively, were reported in the Pycnogenol group, whereas the placebo group showed no significant changes. The dosage and frequency of NSAIDs or COX-2 inhibitors increased in placebo group, which were significantly less in Pycnogenol group.
Another study also found Pycnogenol reduced the need for anti-inflammatory drugs, which the researchers noted also reduced treatment costs and side effects.36 This double blind, placebo-controlled study found oral capsules (100 mg/d) of Pycnogenol for three months decreased WOMAC scores by 56 percent in the treatment group of OA patients versus 9.6 percent in the placebo group. Walking distance in the treadmill test was prolonged from 68 minutes at the start to 198 minutes after the three-months treatment, while, under placebo, the increase was from 65 minutes to 88 minutes. Drug usage also decreased by 58 percent in the treatment group versus 1 percent under placebo. GI complications decreased by 63 percent in the treatment group, but only 3 percent under placebo. Overall, treatment costs were reduced significantly compared with placebo.
In a subset of the previous studys OA patientsthose with elevated CRP and plasma-free radicalsPycnogenol significantly decreased plasma free radicals to 70.1 percent of baseline values, and decreased plasma CRP levels (from baseline 3.9 mg/l to 1.1 mg/l); the control group had initial values of 3.9 mg/l, which decreased to 3.6 mg/l.37 The CRP decrease in the Pycnogenol was statistical significant as compared to the control group.
Next Page: Botanicals (cont.)
Bonus: Chart - Round Up of Joint Health Ingredient Studies
Another double blind, placebo-controlled, randomly allocated trial found knee OA patients reported an improvement of WOMAC index after supplementing with Pycnogenol, and a significant alleviation of pain by VAS, where the placebo group experienced no effect.38 Also, the use of NSAIDs diminished in the Pycnogenol group, but increased under the placebo.
Another botanical, a patented hops extract (as Perluxan®, from Pharmachem) available in softgels (from Soft Gel Technologies), significantly improved parameters of OA pain, including mean pain relief while in bed, sitting, lying and walking on a flat surface. The patients, who took 1 g/d for 14 days in the Pharmachem Labs study, also reduced their use of rescue medication compared to the placebo group. The double blind, randomized trial reported Perluxan intake showed a fast-acting effect on mean pain relief; significant improvement over placebo could be measured two hours after the first ingestion. A second double-blind, randomized, parallel design trial was conducted on 19 healthy subjects and found Perluxan either in a 450-mg/d softgel or a capsule containing hops resin converted to powder (300 mg 4x/d) was as effective as 400 mg/d ibuprofen at inhibiting COX-2, but had significant COX-1 sparing activity over a nine-hour period. However, the softgel had a faster onset of action and gradually reduced pain-causing enzymes over the period of the study.
Curcumin, the principal curcuminoid of the popular Indian spice turmeric (Curcuma longa), which is a member of the ginger (Zingiber officinalis) family, is a the natural phenols that is responsible for the yellow color of the spice. In 2005, University of Texas, Houston, researchers noted turmeric has been used to treat different inflammatory diseases in Ayurveda and in traditional Chinese medicine for thousands of years.39 They said curcumin was active component of turmeric responsible for this activity, and modern science has revealed that curcumin mediates its effects by modulation of several important molecular targets, including transcription factors (e.g., NF-kappaB, AP-1, Egr-1, beta-catenin and PPAR-gamma), enzymes (e.g., COX2, 5-LOX, iNOS, and hemeoxygenase-1), cell cycle proteins (e.g., cyclin D1 and p21), cytokines (e.g., TNF, IL-1, IL-6, and chemokines), receptors (e.g., EGFR and HER2), and cell surface adhesion molecules. Because it can modulate the expression of these targets, they said curcumin is now being used to treat a number of diseasing including OA.
A 2009 study from Bangkok reported Curcuma domestica, at 2 g/d, was as effective as 800 mg/d of ibuprofen in the treatment of knee OA .40 An extract of Indian and Javanese turmeric, Curcuma domestica and Curcuma xanthorrhiza respectively, was helpful to dogs with OA in a 2003 randomized, double blind, placebo-controlled, parallel group clinical trial, as supplementation for eight weeks increased their peak vertical force compared to placebo.41 And, more recently, a 2011 review from the University of Montreal reported curcumin, along with other natural health products, such as epigallocatechin- 3-gallate and resveratrol, suppressed multiple inflammatory and catabolic molecular mediators of both OA and RA.42
Next Page: Creatine and MSM
Bonus: Chart - Round Up of Joint Health Ingredient Studies
Creatine
Kre-Celazine® (from All American Pharmaceutical), a combination of esterified fatty acid carbons and creatine, is thought to enhance the lipid structure of the cell membrane, enabling the cells to repair and regenerate and thus reducing inflammation and pain. All American Pharmaceutical said Kre-Celazine inhibits AA and decreases the pro-inflammatory effects of other fatty acids. A 2009 study reported Kre-Celazine exerted its greatest impact on areas of inflammation/pain in the extremities, as well as in the neck and shoulder region. In the study, 35 subjects were divided into two groups: group A received Kre-Celazine for 30 days, while group B took a placebo.43 Results indicated approximately 100 percent of ankle/foot pain, 80 percent to 85 percent of neck/ shoulder/elbow/wrist and hand pain, and 71 percent of knee pain respondents in group A rated their compound better than/as good as a prescription product in its ability to reduce/eliminate pain. Hip and back pain scores for Group A were no better than placebo scores. Group A experienced a modest increase in mobility (35 percent), but no measurable increase in range of motion over group B.
An additional unpublished study from 2007 performed by BioCeutical Research and Development Laboratory, Billings, MT, reported 12 out of 12 subjects who had arthritis, joint pain and inflammation said they experienced some to significant benefits from taking Kre-Celazine for four weeks over conventional prescription and OTC arthritic and pain drugs. All of the subjects also reported significant benefits over various health store products such as glucosamine and methylsulfonylmethane (MSM).
MSM
As noted in the Kre-Celazine study, MSM, an organosulfur compound, has been known for its joint health promotion, especially in combination with glucosamine. MSM (3 g twice/d) improved symptoms of pain and physical function in patients with knee OA pain without major adverse events in a study from Southwest College Research Institute, Tempe, AZ.44 The randomized, double blind, placebo-controlled trial included 50 men and women, aged 40 to 76 years. Compared to placebo, MSM produced significant decreases in WOMAC pain and physical function impairment. No notable changes were found in WOMAC stiffness and aggregated total symptoms scores. MSM also produced improvement in performing activities of daily living when compared to placebo.
And a 2004 study from India found adding MSM and glucosamine produced an analgesic and anti-inflammatory effect in OA patients.45 Combination therapy showed better efficacy in reducing pain and swelling and in improving the functional ability of joints than the individual agents. Patients with mild to moderate OA (n=118) were randomized to receive either 500 mg of glucosamine, 500 mg of MSM, a combination of 500 mg of glucosamine and 500 mg of MSM, or placebo capsules three times daily for 12 weeks. Glucosamine, MSM and their combination significantly improved signs and symptoms of OA compared with placebo. MSM significantly decreased the mean pain index from 1.53 +/- 0.51 to 0.74 +/- 0.65, and combination treatment resulted in a more significant decrease in the mean pain index (1.7 +/- 0.47 to 0.36 +/- 0.33). After 12 weeks, the mean swelling index significantly decreased with glucosamine and MSM, while the decrease in swelling index with combination therapy was greater (1.43 +/- 0.63 to 0.14 +/- 0.35) after 12 weeks.
No matter how many joints a person hasbe it 230 or 360, he has plenty of options when it comes to addressing joint pain. With the side effects of prescription and OTC drugs, it's a good thing natural ingredients offer a way to soothe inflammation and reduce cartilage decline in a scientifically proven manner.
Next Page: References
Bonus: Chart - Round Up of Joint Health Ingredient Studies
References for "Bending the Rules" by Sandy Almendarez
1. Singh G. Recent considerations in nonsteroidal anti-inflammatory drug gastropathy. Am J Med. 1998 Jul 27;105(1B):31S-38S.
2. Reginster JY et al Long-term effects of glucosamine sulphate on osteoarthritis progression: a randomised, placebo-controlled clinical trial. Lancet. 2001 Jan 27;357(9252):251-6.
3. Herrero-Beaumont G et al. Glucosamine sulfate in the treatment of knee osteoarthritis symptoms: a randomized, double-blind, placebo-controlled study using acetaminophen as a side comparator. Arthritis Rheum. 2007 Feb;56(2):555-67.
4. Towheed TE et al. Glucosamine therapy for treating osteoarthritis. N Engl J Med. 2006 Feb 23;354(8):795-808.
5. Vlad SC et al. Glucosamine for pain in osteoarthritis: why do trial results differ? Arthritis Rheum. 2007 Jul;56(7):2267-77.
6. Bourgeois P et al. Efficacy and tolerability of chondroitin sulfate 1200 mg/day vs chondroitin sulfate 3 x 400 mg/day vs placebo. Osteoarthritis Cartilage. 1998 May;6 Suppl A:25-30.
7. Uebelhart D et al. Intermittent treatment of knee osteoarthritis with oral chondroitin sulfate: a one-year, randomized, double-blind, multicenter study versus placebo. Osteoarthritis Cartilage. 2004 Apr;12(4):269-76.
8. Leeb BF, et al. A metaanalysis of chondroitin sulfate in the treatment of osteoarthritis. J Rheumatol. 2000 Jan;27(1):205-11.
9. Bruyere O, Reginster JY. Glucosamine and chondroitin sulfate as therapeutic agents for knee and hip osteoarthritis. Drugs Aging. 2007;24(7):573-80.
10. ANational Center for Complimentary and Alternative Medicine. The NIH Glucosamine/Chondroitin Arthritis Intervention Trial (GAIT). J Pain Palliat Care Pharmacother. 2008;22(1):39-43.
11. Clegg D, et al. Glucosamine, chondroitin sulfate, and the two in combination for painful knee osteoarthritis. N Engl J Med. 2006 Feb 23;354(8):795-808.
12. Sawitzke AD et al. Clinical efficacy and safety of glucosamine, chondroitin sulphate, their combination, celecoxib or placebo taken to treat osteoarthritis of the knee: 2-year results from GAIT. Arthritis Rheum. 2008 Oct;58(10):3183-91.
13. McNeil JD. Intra-articular hyaluronic acid preparations for use in the treatment of osteoarthritis. Int J Evid Based Healthc. 2011 Sep;9(3):261-4. doi: 10.1111/j.1744-1609.2011.00216.x.
14. Kalman DS et al. Effect of a natural extract of chicken combs with a high content of hyaluronic acid (Hyal-Joint) on pain relief and quality of life in subjects with knee osteoarthritis: a pilot randomized double-blind placebo-controlled trial. Nutr J. 2008 Jan 21;7:3.
15. Sato T, Iwaso H. An effectiveness study of hyaluronic acid [Hyabest®(J)] in the treatment of osteoarthritis of the knee on the patients in the United States. J New Rem Clin. 2009;58(3).
16. Barnett ML et al. Treatment of rheumatoid arthritis with oral type II collagen. Results of a multicenter, double-blind, placebo-controlled trial. Arthritis Rheum. 1998 Feb;41(2):290-7.
17. Barnett ML, Combitchi D, Trentham DE. A pilot trial of oral type II collagen in the treatment of juvenile rheumatoid arthritis. Arthritis Rheum. 1996 Apr;39(4):623-8.
18. Crowley DC et al. Safety and efficacy of undenatured type II collagen in the treatment of osteoarthritis of the knee: a clinical trial. Int J Med Sci. 2009 Oct 9;6(6):312-21.
19. Bagchi D et al. Effects of orally administered undenatured type II collagen against arthritic inflammatory diseases: a mechanistic exploration. Int J Clin Pharmacol Res. 2002;22(3-4):101-10.
20. Deparle LA et al. Efficacy and safety of glycosylated undenatured type-II collagen (UC-II) in therapy of arthritic dogs. J Vet Pharmacol Ther. 2005 Aug;28(4):385-90.
21. D'Altilio M et al. Therapeutic Efficacy and Safety of Undenatured Type II Collagen Singly or in Combination with Glucosamine and Chondroitin in Arthritic Dogs. Toxicol Mech Methods. 2007;17(4):189-96.
22. Espersen GT et al. Decreased interleukin-1 beta levels in plasma from rheumatoid arthritis patients after dietary supplementation with n-3 polyunsaturated fatty acids. Clin Rheumatol. 1992 Sep;11(3):393-5.
23. Faarvang KL et al. [Fish oils and rheumatoid arthritis. A randomized and double-blind study].[Article in Danish] Ugeskr Laeger. 1994 Jun 6;156(23):3495-8.
24. Nielsen GL et al. The effects of dietary supplementation with n-3 polyunsaturated fatty acids in patients with rheumatoid arthritis: a randomized, double blind trial. Eur J Clin Invest. 1992 Oct;22(10):687-91
25. Volker D et al. Efficacy of fish oil concentrate in the treatment of rheumatoid arthritis. J Rheumatol. 2000 Oct;27(10):2343-6.
26. Sundström B et al. Supplementation of omega-3 fatty acids in patients with ankylosing spondylitis. Scand J Rheumatol. 2006 Sep-Oct;35(5):359-62.
27. Hansen GV et al. Nutritional status of Danish rheumatoid arthritis patients and effects of a diet adjusted in energy intake, fish-meal, and antioxidants. Scand J Rheumatol. 1996;25(5):325-30.
28. Ulven SM et al. Metabolic effects of krill oil are essentially similar to those of fish oil but at lower dose of EPA and DHA, in healthy volunteers. Lipids. 2011 Jan;46(1):37-46. Epub 2010 Nov 2.
29. Deutsch L. Evaluation of the effect of Neptune Krill Oil on chronic inflammation and arthritic symptoms. J Am Coll Nutr. 2007 Feb;26(1):39-48.
30. Lee SJ et al. Astaxanthin inhibits nitric oxide production and inflammatory gene expression by suppressing I(kappa)B kinase-dependent NF-kappaB activation. Mol Cells. 2003 Aug 31;16(1):97-105.
31. Ohgami K et al. Effects of astaxanthin on lipopolysaccharide-induced inflammation in vitro and in vivo. Invest Ophthalmol Vis Sci. 2003 Jun;44(6):2694-701.
32. Burnett, B et al. A Medicinal Extract of Scutellaria baicalensis and Acacai catechu Acts as a Duel Inhibitor of coclooxygenase and 5-Lipoxyygenase to Reduce Inflammation J Med Food 2007;10(3)
33. Burnett, B et al. Safety Evaluation of a Combination, Defined Extract of Scutellaria baicalensis and Acacia catechu. Journal of Food Biochemistry 2007;797825.
34. Grimm, T et al. Inhibition of NF-B activation and MMP-9 secretion by plasma of human volunteers after ingestion of maritime pine bark extract (Pycnogenol) Journal of Inflammation 2006;3:1
35. Reza Farida, R et al. Pycnogenol supplementation reduces pain and stiffness and improves physical function in adults with knee osteoarthritis Nutrition Research 2007;27(692697).
36. Belcaro, G. et al. Treatment of Osteoarthritis with Pycnogenol®.The SVOS (San Valentino Osteo-arthrosis Study). Evaluation of Signs, Symptoms, Physical Performance and Vascular Aspects. Phytother. Res. 2008;(22)518523
37. Belcaro G et al. Variations in C-reactive protein, plasma free radicals and fibrinogen values in patients with osteoarthritis treated with Pycnogenol.(R). Redox Report. 2008;13(6)271-76.
38. Cisar P et al. Effect of pine bark extract (Pycnogenol) on symptoms of knee osteoarthritis. Phytother Res. 2008 Aug;22(8)1087-92.
39. Shishodia S, Sethi G, Aggarwal BB. "Curcumin: getting back to the roots." Ann N Y Acad Sci. 2005 Nov;1056:206-17.
40. Kuptniratsaikul V et al. "Efficacy and safety of Curcuma domestica extracts in patients with knee osteoarthritis." J Altern Complement Med. 2009 Aug;15(8):891-7.
41. Innes JF et al. "Randomised, double-blind, placebo-controlled parallel group study of P54FP for the treatment of dogs with osteoarthritis." Vet Rec. 2003 Apr 12;152(15):457-60.
42. Khalifé S, Zafarullah M. "Molecular targets of natural health products in arthritis." Arthritis Res Ther. 2011 Feb 3;13(1):102.
43. Golini J et al. A single-center, double-blind placebo-controlled study to evaluate the efficacy of Kre-Celazine®, an oral buffered creatine-cetylated fatty acid compound, in its ability to reduce site-specific inflammation and pain. JANA. 2009;12(1):20-25.
44. Kim LS et al. "Efficacy of methylsulfonylmethane (MSM) in osteoarthritis pain of the knee: a pilot clinical trial." Osteoarthritis Cartilage. 2006 Mar;14(3):286-94.
45. Usha PR, Naidu MU. "Randomised, Double-Blind, Parallel, Placebo-Controlled Study of Oral Glucosamine, Methylsulfonylmethane and their Combination in Osteoarthritis." Clin Drug Investig. 2004;24(6):353-63.
About the Author(s)
You May Also Like






.png?width=800&auto=webp&quality=80&disable=upscale)