Consumers are confused by omega-3 types and dosages, which could be why so many don’t achieve recommended Omega-3 Index levels, according to a preliminary study conducted by Grassroots Health.

Two years ago, the Organic & Natural Association (O&N) enlisted the partnership of GrassrootsHealth to conduct a nutrient field trail on omega-3 oil and vitamin D. Experts assert that achieving an omega-3 index of 8 to 12 percent is required to reap the full health benefits of eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA).1 However, the majority of the U.S. population is woefully deficient in omega-3 with levels at or below 4 percent.2 Drawing from the 17,000 participants in GrassrootsHealth’s Institutional Review Board (IRB)-approved study, the objective was to determine what is required to achieve effective omega-3 levels and what associated health benefits are derived from achieving optimal levels.
Approximately 1,200 people participated in this first phase of the initiative, with roughly 500 submitting at least two blood spot tests to measure their omega-3 levels. All study participants were also required to complete a survey with questions ranging from the dose consumed, foods eaten, health issues and health outcomes. The median age of study participants was 59. Sixty percent were female, and 93 percent white, residing in 27 countries worldwide, approximately 95 percent of whom resided in the United States or Canada. Preliminary analysis of the nutrient field trial provided insight on omega-3 intake and health outcomes. More importantly, it articulated what we don’t know about the dose response and effectiveness of omega-3.
GrassrootsHealth has drawn the following summary statements from the preliminary findings:
Omega-3 utilization is scattered across a host of products and types of omega-3;
Labels on products are confusing to almost all;
Serving size/dose doesn’t necessarily match the reality of the dose-response curve, which could have major implications for manufacturers and distributors, and
All nutrients need large population size databases to test dose response of their products.
Consumer confusion regarding what kind of omega-3 to take, how much to take, or if it makes a difference when and what you take it with, has been bandied about for years. The study provided this insight on purchasing habits; a total of 494 different omega-3 supplements were used by the participants during the two-year study, representing 236 different brands. Also interesting to note, 17 percent of study enrollees take two or more omega-3 supplements, and 2 percent take three or more. So, while dietary supplement users may be price sensitive, or are responding to recent reports on the effectiveness the wide variety of omega-3 sources, be it cold water fish, plant sources, EPA/DHA or phospholipids, a group of users are intentionally sourcing supplementation from a variety of fish oil, fish oil concentrates and/or krill oil.
Potentially associated with Grassroots’ conclusions around label confusion, significant variability exists in the daily supplemental dosages of study participants, which ranged from 0 mg per day to more than 10,000 mg per day. At the end of two years, only 19 percent of study participants achieved an omega-3 index of 8 percent or higher. Forty-four percent had an index level of 4 to 5.9 percent, and 8 percent were below the 4 percent level. Unlike vitamin D, the variables in how omega-3 is metabolized, vis-à-vis the forms of omega-3 taken, along with the dosage and duration of consumption and the frequency of testing, could all have significant bearing on achieving an omega-3 index level of 8 percent.
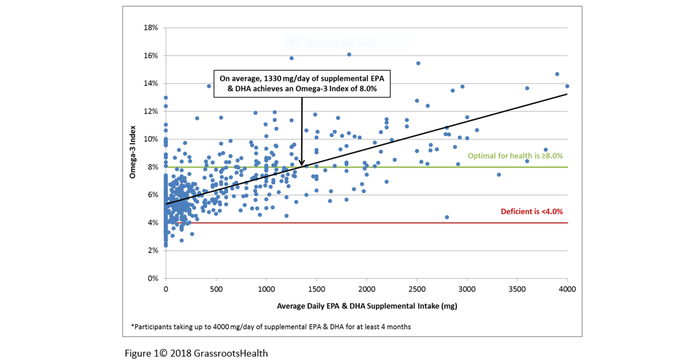
In January 2019, at its annual conference, O&N announced its intention to grow enrollment in the vitamin D/omega-3 study to 5,000 over the next two years. O&N is also in the process of launching a pilot study for 500 participants who will take either krill oil, salmon oil or a combination of the two. Enrollees will test at the beginning and end of a three-month period for both omega-3 and vitamin D. Dosing recommendations for the 500 participants will be made using a preliminary dose-response chart derived from the original study data. The objective for the pilot is to create a dose-response curve that identifies the supplemental intake amount needed for study participants to achieve an omega-3 index of 8 percent.
Building that body of knowledge relating to dose-response is essential to understanding the health outcomes associated with omega-3s. Virtually all randomized controlled trials (RCTs) of nutrients are focused on the assigned study dose, overlooking the level of the nutrient in the body. RCTs are designed for pharmacologic intervention, which can be measured for safety and efficacy since a foreign object (drug) is introduced into the body. All nutrients are efficacious. The better questions, and addressed in nutrient field trials, are for what is the nutrient effective and in what amount?
We are beginning to see relationship between increased omega-3 levels and health conditions.3 However, sufficient data from the GrassrootsHealth study is only available on the power of omega-3 to reduce the number of colds. Those with levels of 8 percent or higher had 38 percent fewer colds than study participants with levels at or below 4 percent. Increasing the study size will enable greater specificity, for a wide array of health conditions, on the impact adequate omega-3 levels have on health status. At the same time, researchers will determine how the interaction of omega-3 and vitamin D relate to health outcomes, a process that can be replicated for the host of nutrients and vitamins consumers are deficient in. Study participants are currently reporting data on 19 nutrients, ranging from vitamin A to zinc. Science-based outcomes, derived by evidence-based consumer decisions will drive industry to create better formulations, and in the end, serve as the vehicle to transform public health policy.
Karen Howard, CEO and executive director of Organic & Natural Health Association has spent more than 30 years working with Congress, state legislatures and health care organizations to develop innovative health care policy and programs. She has held a variety of executive positions, including serving as professional staff for a Congressional committee, and has policy expertise in integrative and complementary medicine, managed care, health care technology and mental health. Prior to Organic & Natural Health, Howard served as executive director for both the American Association of Naturopathic Physicians (AANP) and the Association of Accredited Naturopathic Medical Schools.
References:
Harris W, Von Schacky C. “The Omega-3 Index: a new risk factor for death from coronary heart disease?” Prev Med. 2004 Jul;39(1):212-20
Harris W. “Omega-3 fatty acids.” In: Coates PM, Betz JM, Blackman MR, et al., eds. “Encyclopedia of Dietary Supplements. 2nd ed.” London and New York: Informa Healthcare; 2010:577-86.
Harris W. “The omega-3 index as a risk factor for coronary heart disease.” Am J Clin Nutr. 2008 Jun;87(6):1997S-2002S.
About the Author(s)
You May Also Like





.png?width=800&auto=webp&quality=80&disable=upscale)